Introduction
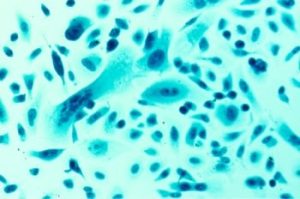
Chimeric antigen receptors (CAR) are proteins that can be expressed by genetically modified T cells (immune response cells) to allow them to react with specified targets. These CAR T cells can currently be used to target some hematological malignancies (cancers that originate in the blood or bone marrow). Research is also currently underway to assess the utility of CAR T cells for targeting autoimmune diseases, solid tumor cancers, as well as liver and cardiac fibrosis [1-3].
Currently, lentiviral or adeno-associated virus (AAV)-mediated gene transfer is the standard method for CAR T cell manufacturing. This method uses viruses to introduce genetic information in T cells in a highly efficient manner. However, there are important issues that surround these manufacturing processes such as excessive CAR expression levels which can lead to cell exhaustion and death [1,4] as well as high production costs . An alternative approach to manufacturing CAR-T cells involves the targeted integration of CAR trans gene into the T cell receptor (TCR) alpha constant chain (TRAC) gene locus using CRISPR/Cas9 technology. Early studies have found that this approach can help solve the problem of excessive expression, provide control of site integration, and allow for the monitoring off-target effects [4].
Studies that have used the TRAC approach have largely relied on transduction with a recombinant adeno-associated virus serotype 6 (rAAV6), meaning that to manufacture CAR T cells at-scale would still be resource heavy and expensive. To solve this issue, Kath et al. aimed to use a virus-vector-free method to integrate CARs into the TRAC locus of T cells. Previous work has successfully generated CAR T cells without relying on viral vectors [5,6]. Kath et al. built upon these findings and optimized this process.
Optimization of virus-free CAR T cell engineering
The first step in optimizing a virus-free CAR T cell engineering workflow using CRISPR/Cas9 technology was to select the correct guide RNA (gRNA) for inserting their CD19-targeting CAR. This first step is important because each gRNA will have a unique off-target profile and because off-target effects can have severe detrimental impacts on cells [7] it is important to choose a gRNA with the lowest amount of these effects as possible. Off-target effects can also be limited by the use of engineered nucleases, such as HiFi-Cas9, which result in lower off-target editing while maintaining on-target potency [8]. Following gRNA and nuclease selection, a donor template for homology-directed repair (HDR) can be designed that has the homology arms aligned with the cut-site.
Then, Kath et al. needed to optimize the conditions in which pre-electroporated T cells were prepared as well as the actual electroporation conditions. More specifically this involved determining how many activated T cells were needed in their electroporation solution, how much Cas9 enzyme, gRNA, and HDR template were needed per electroporation, and determining how different pre-electroporation conditions impacted CAR insertion rates — i.e., T cells stimulation with activator beads vs plate-bound antibodies and commercial electroporation buffer. The researchers determined that plate-bound antibodies in combination with the self-made buffer would result in the ideal CAR insertion rate.
HDR enhancer with dsDNA sensory inhibitor increases knock in efficiency and CAR T cell yield
The next hurdle to overcome was prevent the loss of viability to T cells once the HDR template was transfected. This largely happens as a result of the immune pathways that are present in T cells, when large amounts of DNA are detected, the T cell has natural defense system to prevent that DNA from replicating [9]. To work around this, the researchers temporarily inhibited the cell’s intracellular dsDNA sensors using small molecules. However, their results showed that it was more effective to expose the T cells to smaller amounts of dsDNA during electroporation, rather than to use an intracellular dsDNA sensory inhibitor.
Interestingly, other efforts to increase the efficiency of CAR insert rates showed more promising results. The use of an HDR enhancer showed an average of 38% increase in CAR insertion rate. Further, when the HDR enhancer was combined with the previously tested dsDNA sensory inhibitors, Kath et al. observed an even further increase in TRAC CAR T cell yields. The synergistic enhancement of relative knock-in rate and absolute CAR T cell yield using these two reagents is important because it makes a virus-free approach to CAR T cell engineering much more efficient.
Kath et al. then went on to test the functionality of the TRAC-replaced CAR T cells they generated using their workflow. More specifically, they needed to check that the HDR enhancer and dsDNA sensory inhibitors did not influence the way the CAR T cells behaved in vitro. They found that the CAR T cells generated using the new workflow were as effective as CAR T cells generated without the enhancer and inhibitors. These research findings were further confirmed in vivo using animal models.
Conclusion
The optimization of virus-free TRAC-replaced CAR T cell generation is an important milestone for this field of research. By using commercially available reagents, Kath et al. has provided a workflow that can be easily implemented in labs without needing to rely on time and resource consuming viral production. Further, the use of an HDR enhancer and a dsDNA sensory inhibitor to increase the efficiency of CAR T cell generation without adverse effects to functionality, makes this workflow an attractive alternative to retroviral transduction manufacturing techniques.
Further research is needed to fully evaluate the CAR T cells generated through this method, however the results presented by Kath et al. clearly illustrate the promise that this new workflow has in circumventing the issues currently presented by CAR T cell manufacturing.
References
1. Kath J, Du W, Pruene A, et al. Pharmacological interventions enhance virus-free generation of TRAC-replaced CAR T cells. Mol Ther Methods Clin Dev.. 2022;25:311-330.
2. Aghajanian H, Kimura T, Rurik JG, et al. Targeting cardiac fibrosis with engineered T cells. Nature. 2019;573(7774):430-433.
3. Ellebrecht CT, Bhoj VG, Nace A, et al. Reengineering chimeric antigen receptor T cells for targeted therapy of autoimmune disease. Science. 2016;353(6295):179-184.
4. Eyquem J, Mansilla-Soto J, Giavridis T, et al. Targeting a CAR to the TRAC locus with CRISPR/Cas9 enhances tumour rejection. Nature. 2017;543(7643):113-117.
5. Roth TL, Puig-Saus C, Yu R, et al. Reprogramming human T cell function and specificity with non-viral genome targeting. Nature. 2018;559(7714):405-409.
6. Nguyen DN, Roth TL, Li PJ, et al. Polymer-stabilized Cas9 nanoparticles and modified repair templates increase genome editing efficiency. Nat Biotechnol. 2020;38(1):44-49.
7. Zhang XH, Tee LY, Wang XG, et al. Off-target Effects in CRISPR/Cas9-mediated Genome Engineering. Mol Ther Nucleic Acids. 2015;4(11):e264.
8. Vakulskas CA, Dever DP, Rettig GR, et al. A high-fidelity Cas9 mutant delivered as a ribonucleoprotein complex enables efficient gene editing in human hematopoietic stem and progenitor cells. Nat Med. 2018;24(8):1216-1224.
9. Shirley JL, de Jong YP, Terhorst C, et al. Immune Responses to Viral Gene Therapy Vectors. Mol Ther. 2020;28(3):709-722.
*RUO—For research use only. Not for use in diagnostic procedures. Unless otherwise agreed to in writing, IDT does not intend for these products to be used in clinical applications and does not warrant their fitness or suitability for any clinical diagnostic use. Purchaser is solely responsible for all decisions regarding the use of these products and any associated regulatory or legal obligations.